looking for https://www.drcescolagrande.com
FEDERAL COURT PROCEEDINGS
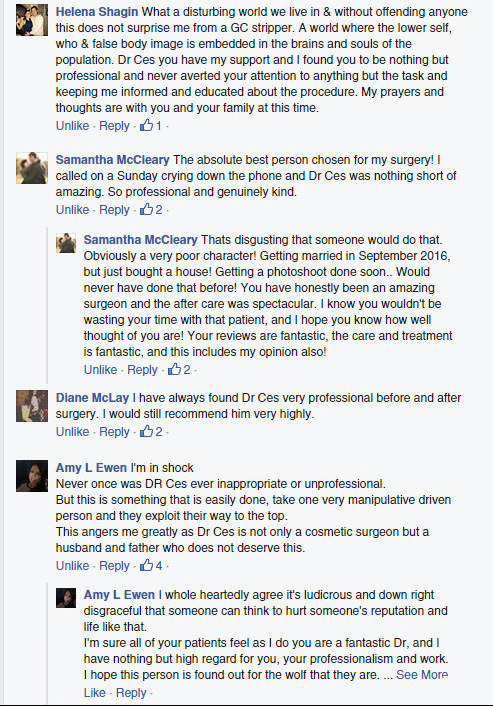
The Federal Court Official Announcement: The proceedings have otherwise settled before trial with an apology to Dr Ces Colagrande and his family. Ms Cassandra (Cassie) McNeill was ordered by the courts to join the proceedings. Dr Colagrande was awarded a monetary payout and pleased with the outcome. He was represented by high profile Sydney Barrister Sue Chrysanthou SC and Blake Fraser, principal of Fraser Lawyers, Mermaid Beach